Detective, the bane of super bacteria is coming.
Original Wuyuan Li Na and other SIFIC infection horizons

Author: Wu Yuan Li Na Jin Wenting Ma Yuyan
Review: Hu Bijie and Pan Jue
First, a brief introduction to medical history
Male, 63 years old, from Shanghai, was admitted to the Infectious Diseases Department of Zhongshan Hospital for the second time on November 23, 2022.
Chief complaint: indwelling catheterization with repeated urine color turbidity for 2 months and then 8 days.
Current medical history:
On September 19, 2022, I went to a hospital in Shanghai for fatigue, anorexia and dysuria. WBC 10.12×10 9/L, N 87.6%, Hb 53g/L, hsCRP 135.22mg/L, ESR 62mm/H, albumin 30.1g/L, Scr 589μmol/L, K 2 were examined. Urine routine: WBC 3892/ul, occult blood 3+/RBC 5579/ul, protein 2+; Chest CT: bilateral pleural effusion, partial atelectasis of lower lobe of both lungs; Abdominal pelvic CT: Bilateral middle and upper ureteral dilatation and renal pelvis and calyceal dilatation, the patch in the right part of calyceal is slightly high density, the bladder wall is thickened, there is a little flocculent blur around the left renal fat sac and ileocecal part, and there is a little effusion in the pelvic cavity. A large amount of turbid urine was drained by indwelling catheter. Urine culture showed that Klebsiella pneumoniae was positive. Considering urinary tract infection, acute kidney injury, hypokalemia and severe anemia, patients were given symptomatic support treatment such as anti-infection, bladder irrigation, antioxidation, potassium supplementation and blood transfusion. The symptoms of patients improved and the urine was slightly clarified. 10-18 Review urine routine: WBC3+, RBC3+, protein 1+, SCR 263 μ mol/L.
I was admitted to our department on October 19, 2022. Blood routine: WBC 5.08X10 9/L, N 66.1%, inflammatory markers: ESR 19mm/H, hsCRP 52.3mg/L, PCT 0.52ng/ml, Scr 257μmol/L, and urine routine: WBC 28493/μ. Urinary color Doppler ultrasound: hydronephrosis, bilateral ureteral dilatation, bladder wall thickening significantly; Abdominal pelvic CT: hydronephrosis of both renal pelvis and ureter, thickening of ureter wall (inflammatory change), inflammatory change of bladder and ureter may be large, the volume of both kidneys increases and the substance is thin. Meropenem 1g q12h is given for empirical anti-infection. Urology consultation considers the acute stage of infection, so it is not suitable to put double J tubes. If necessary, pyelostomy can be done, but it does not improve renal function much. Bladder irrigation is recommended. 10-20 middle-stage urine culture (sampling on October 19): Klebsiella pneumoniae was positive; 10-22 urine culture drug sensitivity: Carbapenem-resistant Klebsiella pneumoniae (CRKP), adjusted to ceftazidime and abamectin 2.5g q12h for anti-infection, and daily bladder irrigation. After treatment, the urine color of the patients gradually became clear, and the urine white blood cell and bacterial count gradually decreased during follow-up. The urine bacterial culture was negative on November 1 and November 4. Check the urine routine on November 09: WBC 28/uL, RBC 4/uL, urine protein+,bacterial count 29/UL;Blood WBC 7.64×10 9/L, N 76.5%, hs-CRP 0.4mg/L, ESR 25mm/H, PCT 0.18ng/mL, Scr 175μmol/L, which were significantly improved compared with those at admission. Stop ceftazidime and abamectin on November 11 and be discharged.
On November 15, 2022, the patient appeared turbid urine again, and there was no fever and other discomfort. On November 23, he was admitted to the hospital for a second diagnosis and treatment.
Past history: In September, 1991, T12-L1 comminuted fracture was treated with internal fixation. After operation, the catheter was retained for half a year due to urinary incontinence, and then the catheter was removed after urination. There was no urinary tract infection during this period. Diabetes for 16 years, insulin therapy, blood sugar control can be; Hypertension for 5 years, oral amlodipine to reduce blood pressure, blood pressure control can be.
Second, the admission examination (admitted on November 23, 2022)
[physical examination]
T: 36.2℃ P: 90 times/min R: 20 times/min BP: 176/105 mmHg.
Stay in bed, feel refreshed and calm, lose weight, and muscle atrophy of lower limbs; Breathing sounds in both lungs are thick, and dry and wet rales are not heard; The rhythm of the heart is regular, the abdomen is soft, without tenderness and rebound pain, without mass, without percussion pain in both kidneys, without tenderness at ureter point and rib and waist point, and the lower abdomen does not touch the enlarged bladder. During indwelling catheterization, the urine in the urine collection bag is turbid and more white flocs are deposited. Limbs are not swollen.
[Laboratory examination]
Blood routine: WBC 7.85×10 9/L, N 81.3%, HB 121g/L, PLT 170×10 9/L.
Urine routine: WBC 2775/μ l; RBC 2/μl, bacterial count: 39879/μl, nitrite positive, leukocyte esterase+++.
Inflammation markers: hs-CRP 17.9mg/L, ESR 68mm/H, PCT 0.12ng/mL.
Biochemistry: ALT/AST 23/21U/L, Alb 47g/L, Scr 199μmol/L, eGFR 30ml/min/1.73m2, na/k 140/5.5mmol/l.
Third, clinical analysis
Characteristics of medical history: middle-aged and elderly male, indwelling catheter, with repeated urinary turbidity and abnormal urine routine. Urine culture showed CRKP one month ago, and it improved after ceftazidime-ababactam treatment, but urine turbidity reappeared three days after drug withdrawal, blood inflammatory index increased, urinary leukocyte and bacterial count increased significantly, and the diagnosis of urinary tract infection was clear. The reasons for short-term recurrence after antibacterial drug treatment improved were considered:
Recurrence of CRKP infection: The patient has been indwelling catheter for 2 months, and there may be biofilm formation of catheter and abnormal urinary tract structure, which makes it difficult to completely eliminate the infection and relapse after stopping taking the drug. Therefore, urine culture and drug sensitivity test can be improved.
New infection: the patient has high risk factors of recurrent urinary tract infection, and the pathogen may be different each time. The patient’s previous CRKP infection treatment was effective, and the possibility of new pathogen infection should be considered in the short term, until the urine culture is perfect and clear.
Multiple infections: patients with abnormal urinary tract structure, indwelling catheter and other risk factors can not be removed, so it is necessary to be alert to the possibility of multiple pathogens including fungi combined with infection, repeat the cultivation of urine bacteria, mycoplasma, fungi and mycobacteria, and improve urine mNGS to help clarify the infected pathogens.
Four, further examination, diagnosis and treatment process and treatment response
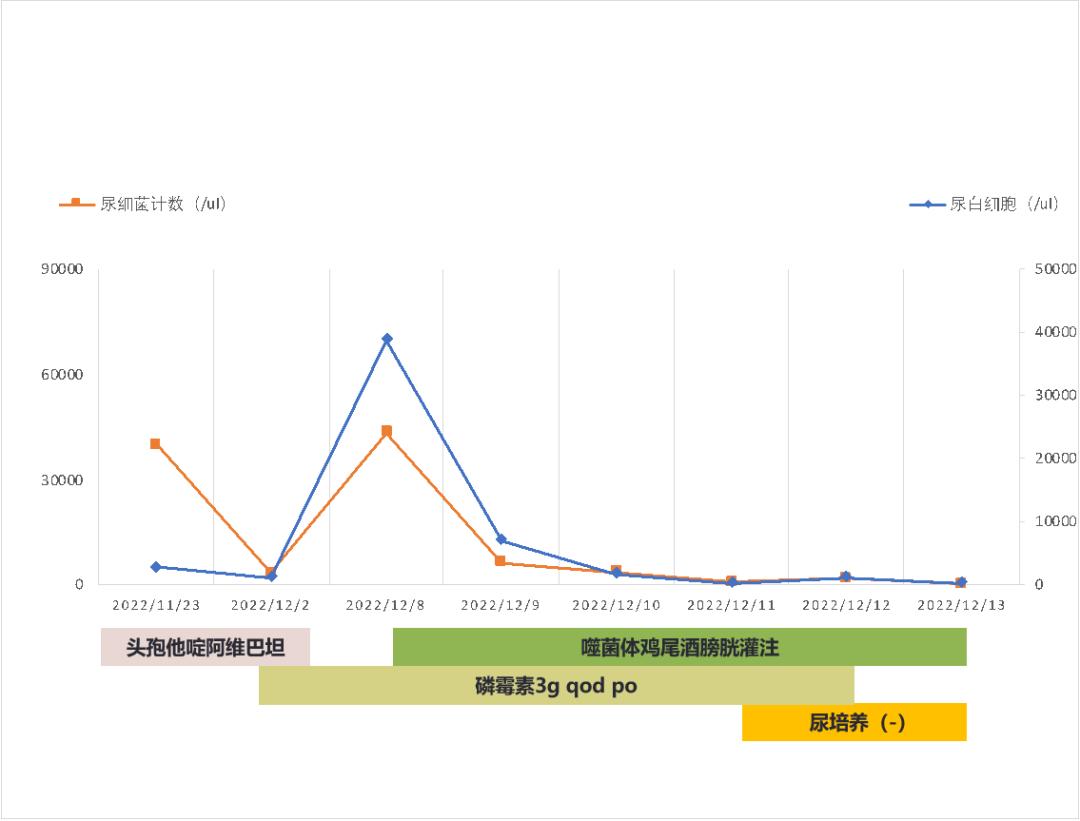
On November 23, 2022, the middle urine smear was used to find bacteria: moderate amount of G- bacilli, and continued ceftazidime and abamectin 2.5g q12h ivgtt for anti-infection and bladder irrigation.
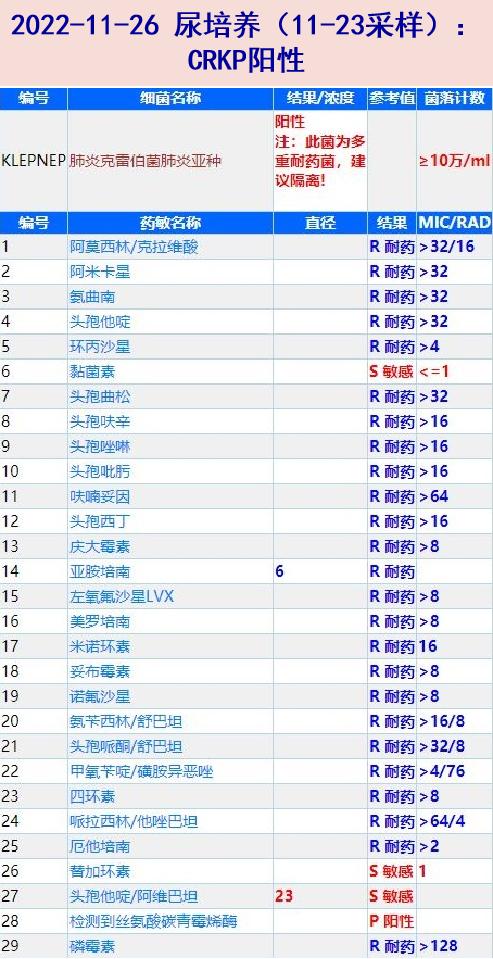
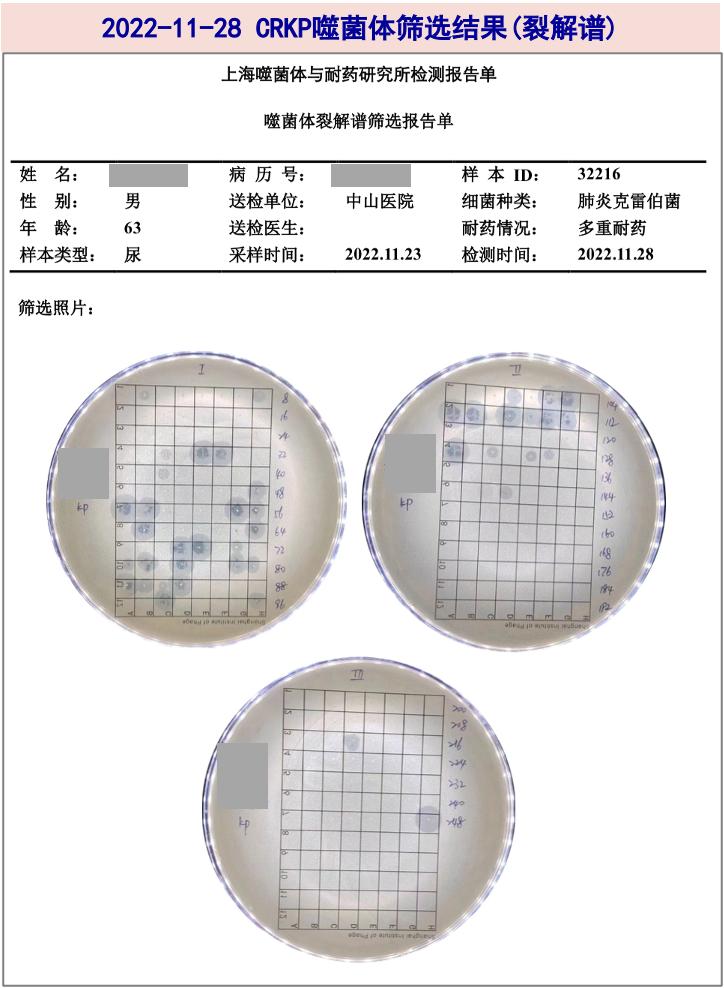
On November 26, 2022, the bacterial drug sensitivity of the middle-stage urine culture (sampling on November 23) was CRKP, ≥ 100,000 /ml, and urine mNGS: a large number of Klebsiella pneumoniae (species strict sequence number: 406,866) was detected.
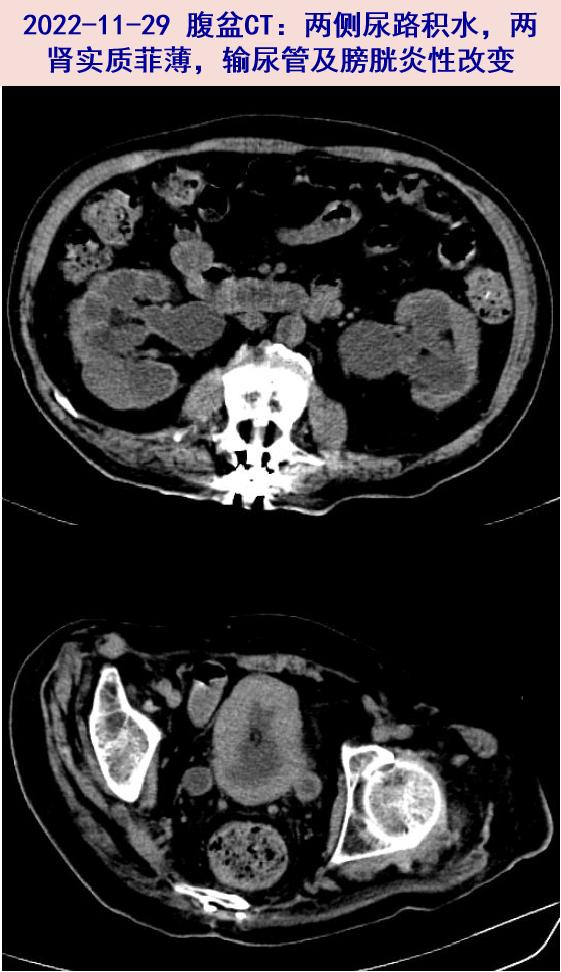
On November 29, 2022, the abdominal and pelvic CT was reexamined: bilateral dilated hydronephrosis accompanied with inflammatory changes of ureter, and the parenchyma of both kidneys was thin, and the inflammatory changes of cystitis might be larger, similar to that of 22-10-20 slices.
November 30, 2022 (sampling on November 29): Enterococcus faecalis was positive. On December 2, according to the drug sensitivity, fosfomycin 3g qod was added orally, and ceftazidime and abamectin were suspended.
Repeated urine cultures on March, April and June, December, 2022: Enterococcus faecalis was positive and CRKP was negative.

On December 8, 2022, the urine WBC was 38738/μ L, and the bacterial count was 43285/μ L; Urine culture: CRKP positive, Enterococcus faecalis negative.
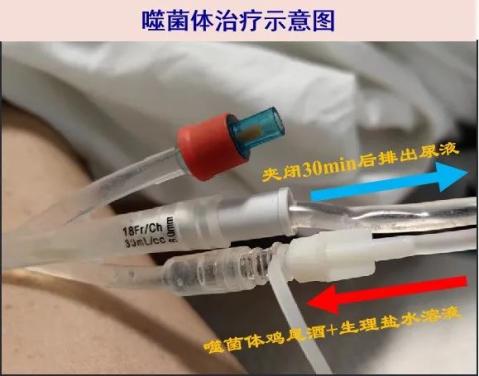
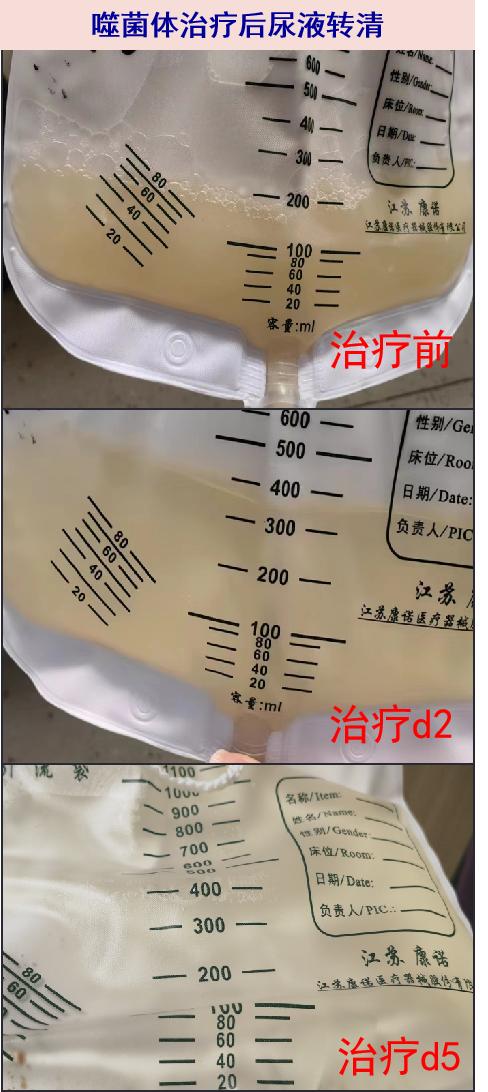
Phage therapy was carried out from the afternoon of December August, 2022: Phage cocktail (composed of 5 strains of Klebsiella pneumoniae phages A103KP172, A106KP176, A121KP192, A49KP106 and A58KP118, 5mL each), injected with 225mL physiological saline (according to the estimated bladder volume), and the total volume was 250mL, and then the catheter was clamped.
Urine routine on the third day of phage treatment on December 11, 2022: white blood cell count: 235/uL, bacterial count: 722/uL;; Urine bacterial culture was negative.
Urine routine on the 5th day of phage therapy on December 13th, 2022: white blood cell count: 279/uL, bacterial count: 92/ul; Urine bacterial culture was negative; Blood WBC 6.35X109/L, N 70%, hs-CRP 0.9mg/L, ESR 26mm/H, and inflammatory index decreased compared with before; Re-examination of urinary color ultrasound showed that bilateral renal pelvis separation and upper ureteral dilatation were better than before (10-20), and the thickness of bladder wall was reduced (12-25mm→13mm).
He was discharged from hospital on December 14, 2022 for follow-up.
V. Final diagnosis and diagnosis basis
Final diagnosis:
Complex urinary tract infection (CRKP, Enterococcus faecalis)
Neurogenic bladder, hydronephrosis and hydroureter (indwelling catheter)
Renal insufficiency
Diagnostic basis:
The patient is a middle-aged and elderly male with neurogenic bladder caused by paraplegia, indwelling catheter, turbid urine with flocs, increased CRP and PCT, significantly increased WBC and bacterial count in urine, repeated CRKP positive in urine culture, positive in enterococcus faecalis, abdominal basin CT: hydronephrosis of renal pelvis and ureter, anti-infection, normal inflammatory markers and urine routine after phage treatment, clear urine and negative urine culture, so complicated urinary tract infection.
The patient suffered from anorexia and dysuria, and the serum creatinine increased obviously. Abdominal CT showed that both kidneys were enlarged, the cortex was thin, and bilateral urinary tract was hydronephrosis. After active treatment such as controlling infection and improving renal function, the serum creatinine decreased, so the diagnosis of renal insufficiency was clear.
Six, experience and experience
Phage is a targeted sterilization virus in nature and a sterilization star in the "pre-antibiotic era". Phage therapy has a history of more than 100 years, but the discovery and application of broad-spectrum antibiotics have gradually marginalized it. With the increasingly serious problem of bacterial drug resistance, phages have once again received attention and become the most promising supplement and alternative therapy for treating superbugs. The clinical application of phage in China is relatively late, but it has developed rapidly in recent years. In 2017, the Shanghai Institute of Phage and Drug Resistance was established, with Professor Hu Bijie as an academic member. Since 2018, the institute has carried out the first clinical trial of phage therapy in China. At present, it has treated nearly 100 patients with drug-resistant bacterial infections from all over the country and accumulated rich clinical experience in phage therapy, which is a leading position in the field of clinical phage therapy in China.
Phage has many advantages, such as host bacteria dependence, targeted specific sterilization, no infection to eukaryotic cells (little influence on normal flora), no influence on bacterial drug resistance, synergy with antibacterial drugs, penetration of biofilm and so on. The cure rate of acute bacterial infection is high, and the therapeutic effect of chronic bacterial infection is no less than that of antibacterial drugs, and the safety of phage treatment is also extremely high. A systematic retrospective study showed that the vast majority of patients who received phage therapy had no or only slight adverse reactions, 86.7% patients’ clinical symptoms improved, and 78.8% patients achieved the eradication of pathogenic bacteria. Our clinical trials also show that more than 70% of patients have achieved good therapeutic effects, and there are no obvious cases of adverse reactions. This patient was repeatedly infected with Klebsiella pneumoniae due to long-term paraplegia, abnormal urinary tract structure, indwelling catheter and other factors. The diagnosis of complicated urinary tract infection was unquestionable, and the choice of antibacterial drugs was limited due to multi-drug resistance and renal insufficiency. Phage therapy is very suitable.
The disadvantages of phage therapy include narrow host spectrum, individualized plan (it is difficult to treat empirically), no unified standard for the best treatment decision, and rapid tolerance. Phage cocktails, combined antibacterial drugs and multiple treatments are usually used in clinic to improve the curative effect. At present, the targeted pathogens of phage therapy in our team mainly include: multi-drug resistant Gram-negative bacteria (Klebsiella pneumoniae, Pseudomonas aeruginosa, Acinetobacter baumannii, Escherichia coli) and Gram-positive bacteria (Staphylococcus aureus, Enterococcus faecalis, Enterococcus faecalis); Covering respiratory system, urinary system, abdominal cavity, bones and joints, skin and soft tissue and other infected sites; Treatment depends on the site of infection, and intravenous application of phage is still being explored. In this case, the patient didn’t have percutaneous nephrostomy because of the little clinical benefit, so he was treated by transurethral bladder perfusion, and the phage could not cover the whole urinary tract evenly. Although the pathogen turned negative in a short period of time and was well tolerated, its long-term curative effect may not be good, and it needs repeated phage treatment.
Phage therapy has huge clinical demand and broad market. In recent years, our team has focused on the clinical application (treatment and prevention and control of nosocomial infection) and basic research of phage therapy, with a view to becoming a powerful weapon to curb drug-resistant bacteria in the future.
references
[1] Uyttebroek S, Chen B, Onsea J, Ruythooren F, Debaveye Y, Devolder D, Spriet I, Depypere M, Wagemans J, Lavigne R, Pirnay JP, Merabishvili M, De Munter P, Peetermans WE, Dupont L, Van Gerven L, Metsemakers WJ. Safety and efficacy of phage therapy in difficult-to-treat infections: a systematic review. Lancet Infect Dis. 2022 Aug; 22(8):e208-e220.
[2] Chegini Z, Khoshbayan A, Taati Moghadam M, Farahani I, Jazireian P, Shariati A. Bacteriophage therapy against Pseudomonas aeruginosa biofilms: a review. Ann Clin Microbiol Antimicrob. 2020 Sep 30; 19(1):45.
[3] Lusiak-Szelachowska M, Weber-Dabrowska B, Gorski A. Bacteriophages and Lysins in Biofilm Control[J]. Virol Sin, 2020,35(2):125-133.
Every Monday night
The Department of Infectious Diseases of Zhongshan Hospital affiliated to Fudan University in Shanghai will be with you!
Photo: Xiaoxiao
Original title: "Detective Case: The Nemesis of Super Bacteria is Coming"
Read the original text


















































